Apolipoprotein B (apob test UK) the Longevity Biomarker
Introduction
Cardiovascular disease is the leading cause of death in the UK and the world. Although in recent times the risk of death has declined in the UK, it remains a primary cause of death as CVD risk can be produced due to other comorbidities such as liver and kidney disease [1]. Moreover, recently cardiovascular risk has not only been limited to an older population but data has emerged expressing the increase in adverse cardiovascular health problems in people aged between 18 and 45 years [2]. Most of these risks are due to unhealthy and extremely sedentary lifestyles with the advancement of technology. Therefore, it has become increasingly evident that diagnosing and early intervention of cardiovascular health may be a high priority. Most common life-threatening heart conditions are due to atherosclerotic diseases which cause a blockage in the coronary arteries of the heart leading to a heart attack. The primary cause of atherosclerotic plaque formation in these blood vessels is increased cholesterol in the body. The major components of the atherosclerotic plaques are lipoproteins of which the apolipoprotein is an integral part. Furthermore, an increase in cholesterol is due to an unhealthy diet, exercise, and in rare instances hereditary. In practice currently, cholesterol levels are advised to be monitored once in 4 to 5 years. However, current diagnostic biomarkers such as total cholesterol and low-density lipoproteins (LDL) are not always reliable in assessing the risk of cardiovascular events. Therefore, alternative diagnostic approaches such as apolipoprotein B are emerging as new targets for better identification and earlier prevention of cardiovascular diseases.
What is Apolipoprotein B (ApoB)?
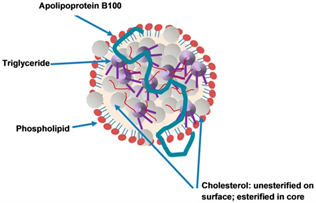
Apolipoprotein is a human lipoprotein that is essential for metabolism in the human body [3, 4]. There are two isoforms of Apo B, which are Apo B-48 and B-100. These isoforms are essential in the metabolism and synthesis of very low-density lipoproteins (VLDL) and low-density lipoproteins (LDL) in the liver [4]. Apolipoprotein is largely responsible for the metabolism and transport of lipoproteins [5]. Apolipoprotein also serves as a framework for maintaining the structural integrity of lipoprotein [6]. Figure 1 below illustrates the example of an Apo B 100 and its importance in the structure of a lipoprotein particle.
Importantly, Apo B is vital in the homeostasis of lipid metabolism as it plays a crucial role in VLDL and chylomicron synthesis. However, high levels of Apo B in the serum can lead to increased risk of atherosclerotic events and mortality [7]. Moreover, it has also been noted that apolipoprotein is essential for the atherogenesis and its presence in the subendothelial cells the blood vessels aids this formation [8]. Therefore, high levels of Apo B, LDL and cholesterol are associated with a higher risk of atherosclerosis and inversely lower Apo B levels may prevent cardiovascular events [9]. Based on this evidence it maybe beneficial to explore whether Apo B is better and more accurate method of preventing and diagnosing cardiovascular risk.
Why ApoB is a better biomarker for cardiovascular disease?
It is a well-established fact that high cholesterol is directly associated with adverse cardiovascular risks. Conventionally, in clinical practice in the UK and globally, the use of LDL and total cholesterol is commonly practiced in diagnosing hypercholesterolaemia (high cholesterol) and its risk in cardiovascular disease such as myocardial infarction [10]. Although it is generally reliable to measure serum LDL levels, certain evidence suggests that it may not always have an accurate reading or give the full picture of risk to the heart especially in patients with other health conditions like diabetes [11]. Therefore, the use of Apo B measurements has recently been explored to combat the issue of these inaccuracies with just measuring LDL and total cholesterol. As stated earlier, Apo B plays a crucial role in the secretion of VLDL and LDL in the liver and subsequently these have an increased risk of atherosclerosis, which results in fatal heart conditions [12]. Interestingly, evidence also suggests that approximately half of the patients with recurrent coronary heart disease have normal LDL and total cholesterol levels. However, these patients are still at an increased risk of cardiovascular events. Therefore, considering that an Apo B molecule is present in every atherogenic particle, it has been proposed as a better indicator for cardiovascular and atherosclerotic diseases by researchers [13]. The primary reason for this is due the fact that 90% of Apo B particles are found in LDL, in contrast LDL particles vary in size and do not always correlate in accurate cholesterol levels [14]. Recent studies have shown that Apo B is a better indicator of risk of cardiovascular diseases such as myocardial infarction in both males and females irrespective of age [15]. This is likely due to the fact that Apo B is a measurement of the total number of atherogenic particles such as LDL, VLDL, IDL, chylomicrons and chylomicrons remnants, whereas LDL cholesterol is a measurement of the mass of total LDL cholesterol only [7]. In the Copenhagen City Heart study, it was noted that when comparing LDL and Apo B as predictors of risk for cardiovascular events in both male and females, Apo B showed a superior prediction of CVE in comparison with LDL [16]. Therefore, the potential of Apo B as a diagnostic predictor of cardiovascular disease should not be underestimated.
ApoB blood test
It has become evident that LDL measurement alone, especially in patients with insulin resistance such as diabetes, gives an inaccurate prediction of cardiovascular adverse events. Some studies have suggested that compared with LDL, Apo B is a much better predictor of cardiovascular disease and may the future of diagnostic and preventive cardiovascular medicine [17]. After scrutinising evidence of the importance of Apo B, at Span clinic we include the Apo B blood test along with other extensive lipid profile tests to give a much clearer picture and accurate quantification of cardiovascular risk. The importance of this test has been noted as lower levels of Apo B are associated with lower all-cause mortality risks [18]. Hence, Apo B as biomarker for predicting cardiovascular events has been gaining rapid popularity and now you can book at Span clinic and have a comprehensive blood panel which includes apob.
How to lower ApoB?
Lower Apo B levels is associated with decreased risk of cardiovascular events. Currently there are two major categories of Apo B reduction. These can be divided into lifestyle changes and pharmacological treatments.
Lifestyle
Evidence suggests that lifestyle changes such as healthy eating and physical activity is associated with an increase in insulin like growth factor (IGFBP-2), which results in a decrease in circulating Apo B proteins [19]. Subsequently, this results in decreased risk of cardiovascular disease. Therefore, a healthy diet and exercise regimen can combat Apo B increase in the human body.
Pharmacological
Current evidence suggests that the current therapies for lowering cholesterol such as the statins and the non-statin treatments such as the PCSK-9 inhibitors work efficiently in reducing the Apo B levels in the blood. Studies have shown that in clinical trials statins and fibrates greatly reduced the Apo B levels and reduced the risk of cardiovascular events [18]. In some rare cases surgical options also showed a good reduction in Apo B levels.
Therefore, the reduction of Apo B levels can be achieved by the above-mentioned options, which are not too dissimilar to existing treatments for lowering cholesterol. The important difference is that Apo B is a much better predictor of cardiovascular risks and early intervention due to the Apo B test may reduce the number of deaths due to cardiovascular diseases.
References